
While neonatal echocardiographers may not need to precisely define the nature of a structural abnormality, they DO at least need to be able to appreciate that there IS an abnormality.
Therefore all infants should have a complete set of standard views carried out at their first echo.
We will add to the list over time, or feel free to email in your suggested diagnoses or images.
Transposition is one of the core neonatal diagnoses to grasp. Correct diagnosis is critical as antenatal diagnosis can be difficult, and infants often present shocked and in need of resuscitation and urgent cardiology intervention (including emergency balloon atrial septostomy).
In the normal heart the aorta and pulmonary trunk can readily be seen to cross. From the parasternal long axis view this can be demonstrated by visualising the aorta heading parallel to the tranducer, and then sweeping to look to the subjects left shoulder where the pulmonary trunk is visible.
This crossing can also be seen from the apical four chamber view. A further check comes from demonstrating bifurcation of the vessel leaving the right ventricle.
In the case of transposition the pulmonary trunk and aorta can be seen to be parallel in the long axis view. This is NEVER NORMAL!
Also the vessel exiting the right ventricle does not bifurcate, rather it can be seen to become the aortic arch.
If you suspect transposition urgent referral to a cardiologist is mandatory. They may need to perform an urgent balloon atrial septostomy, so try to estimate whether there is mixing at the atrial level.
This case emphasises the need to carry out a full structural assessment from each of the 7 core views.
Had one looked only from the apical 4 chamber view this child’s heart may have appeared normal.
However from the parasternal long axis view it is obvious that there is a large VSD.
While VSDs are often an isolated finding, they should also ALWAYS be thought of as a marker for other structural cardiac pathology. In this case interrogation of the right ventricular outflow tract reveals turbulent flow across the pulmonary valve
And on the subcostal view the aorta can clearly be seen to be over-riding the VSD.
From the 4 chamber view it is obvious that this heart is not normal. The atrio-ventricular valve leaflets do not appear to show two normal mitral and tricuspid valves
If you're not sure, compare the image above to a normal 4 chamber view:
Using colour Doppler it appears that both ventricles are filling from a single atrium.
And examining the outflow tracts both again seem to come from the right ventricle. In this case the outflow tract to the left of the screen (in blue) shows relatively laminar flow, the second tract to the right shows turbulent flow (in orange).
Again, in our view neonatal echocardiographers should be focussed on appreciating normality (and abnormality) rather than precisely delineating the exact structural nature of a lesion. In this child for example, if the presentation was cyanosis after birth, management should be initiation of a prostglandin infusion, and urgent discussion with a cardiologist, rather than prolonged attempts to describe a complex abnormal morphology.
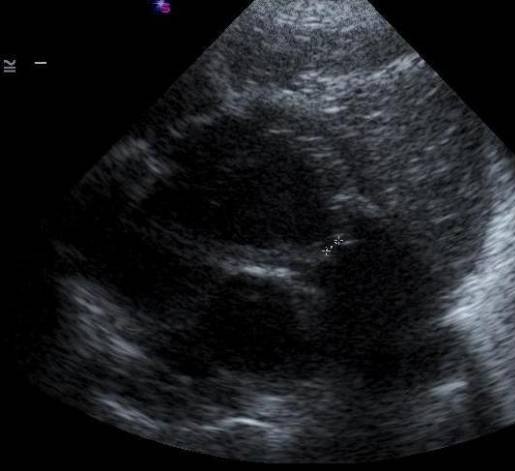
From this 4 chamber view it is clear that the heart is abnormal. Whereas the aortic valve should normally be widely patent with visible leaflet motion the valve looks very narrow, and the leaflet motion is barely visible.
Such gross anatomical defects are often not isolated - in this case the arch view demonstrates that the entire ascending aorta is hypoplastic.
Significant pulmonary stenosis can be readily detected from either the long axis or short axis views. From the long axis view tilt to look towards the subject’s left shoulder. In this infant the pulmonary valve leaflets look thickened and relatively immobile.
This finding is confirmed from a parasternal short axis view
Where the valve orifice measures less than 2mm.
Again a simple four chamber view instantly demonstrates an abnormality. There is no apparent motion of the tricuspid valve, and there is a large VSD.