POCUS Lung

Huge thanks to Dr Ben Ficial and Dr Iuri Corsini for all their hard work on this section of the website. For more information see also their excellent 2020 review article on neonatal lung ultrasound (Corsini et al, Pediatric Pulmonology 2020:1-13):
Why Lung Ultrasound?
Lung ultrasound (LUS) has been increasingly used as a point‐of‐care method in recent years, particularly in the evaluation of critically ill patients, in whom timely diagnosis and treatment are of paramount importance. LUS has numerous advantages compared to traditional imaging tools (CXR): - it is quick - it is portable - it does not use ionizing radiation - it is performed by the same physician who cares for the patient, thus allowing easier integration with clinical findings - it can be repeated to follow the progress of the disease and the response to treatment. - it is a relatively easy-to-learn technique There is a large body of evidence that LUS has an excellent diagnostic effectiveness com- pared to CXR, not only in adults and children, but also in neonates.Who Should Perform Lung Ultrasound?
We think every neonatologist, neonatal trainee and practitioner should have at least a basic knowledge of LUS. LUS, as with many pointof care ultrasound techniques is becoming “the new stethoscope" Formal training and accreditaiton processes are under development internationally, and a growing number of clinical guidelines and training courses are available. This page is designed as an introduction to the technique, but should of course not be used in isolation. Collaboration with pediatric radiologists remain of paramount importance to gain experience in LUS. It's vital to have local guidance, credentialing and quality asurance. We acknowledge that all this will takes some hard work, but we promise it's worth it! LUS has a relatively short learning curve compared to other POCUS modalities like cardiac US. Even if you have little experience, believe in what you see! High agreement between novice and expert physicians has been reported.When to Perform Lung US in the NICU?
LUS has the potential to be used as a first imaging tool in the assessment of a neonate with respiratory distress. So, in time we can consider performing LUS in every neonate admitted for respiratory distress or with a sudden deterioration of respiratory status. The aim is not to eliminate conventional radiologic techniques but rather to complement their use. - reducing their use to avoid unnecessary exposure to ionizing radiations when possible.
Experienced operators can also use LUS to monitor the progress of respiratory illness, to guide treatment (i.e. need of surfactant, weaning of mechanical ventilation, lung recruitment) and to perform invasive procedures (chest tube insertion, needle aspiration).
How to Perform Lung US in the NICU?
LUS can be performed using virtually any commercially available 2‐D scanner. There is no need for a second harmonic or Doppler imaging mode, so even older ultrasound machines can be used. High‐frequency micro-linear probes (i.e. hockey stick probes) are more suitable for LU in neonates and infants, although also other probes can be used. A growing number of handheld probes with linear transducers are available - these seem particularly suitable for brief point of care lung imaging. Care should be taken to ensure the infant is comfortable and placed in the supine position to allow assessment of the anterior and lateral chest. To examine the back, the infant should be placed on their side or prone. Although recently published guidelines on LUS in neonates recommended examination of the entire chest (anterior, lateral, and posterior), there is still a paucity of data to support this practice. Therefore, to minimize handling of the most unstable neonates, it may be advisable not to alter the neonate's position exclusively to perform LUS. An exception might be necessary when localized or heterogeneous lung conditions are suspected.
To standardize the technique, divide the chest surface into three regions by using the anterior and posterior axillary lines as boundaries:
1) Anterior region, from parasternal to anterior axillary line
2) Lateral region, from anterior to posterior axillary line
3) Posterior region, from posterior axillary to paravertebral line.
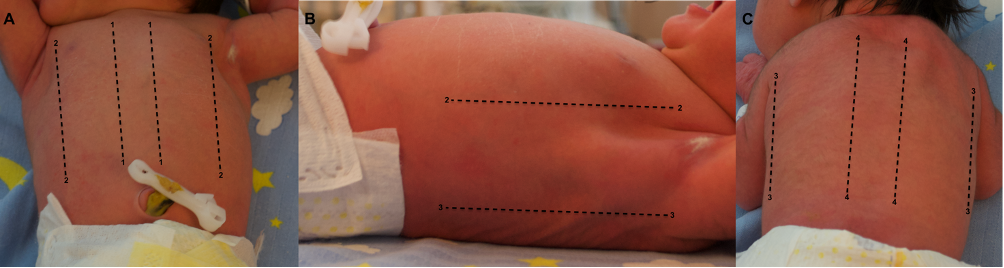 For Lung ultrasound the neonatal chest divided into three zones. (1) Anterior from parasternal to anterior axillary line; (2) lateral from anterior to posterior axillary line; (3) posterior from posterior axillary to paravertebral line.
First perform longitudinal scanning. Place the probe perpendicular to the ribs and slide it progressively from the midline toward the lateral line. After examining the anterior upper region, move the probe towards the feet to scan the remaining areas of the lungs.
Remember: adjust depth (usually 4 to 5 cm) and position the focus marker at the pleural line level.
For Lung ultrasound the neonatal chest divided into three zones. (1) Anterior from parasternal to anterior axillary line; (2) lateral from anterior to posterior axillary line; (3) posterior from posterior axillary to paravertebral line.
First perform longitudinal scanning. Place the probe perpendicular to the ribs and slide it progressively from the midline toward the lateral line. After examining the anterior upper region, move the probe towards the feet to scan the remaining areas of the lungs.
Remember: adjust depth (usually 4 to 5 cm) and position the focus marker at the pleural line level.
 Then rotate the probe by 90° and move it laterally along the intercostal spaces for transverse scanning. In the case of an emergency situation or in a chronic setting, the examination can be more focused and should be clinically driven.
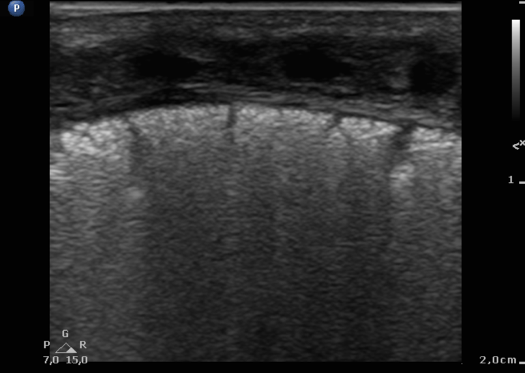
Finally, it is also valuable to evaluate the diaphragm by a subcostal view. Ideally use a micro-convex probe. Place the probe below the xiphoid and tilt it from side to side to scan the diaphragm.
Then rotate the probe by 90° and move it laterally along the intercostal spaces for transverse scanning. In the case of an emergency situation or in a chronic setting, the examination can be more focused and should be clinically driven.
Finally, it is also valuable to evaluate the diaphragm by a subcostal view. Ideally use a micro-convex probe. Place the probe below the xiphoid and tilt it from side to side to scan the diaphragm.
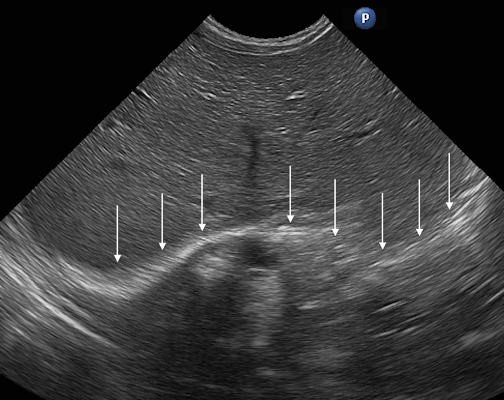 Transverse scan of the abdomen with normal diaphragmatic profile (white arrows).
Transverse scan of the abdomen with normal diaphragmatic profile (white arrows).

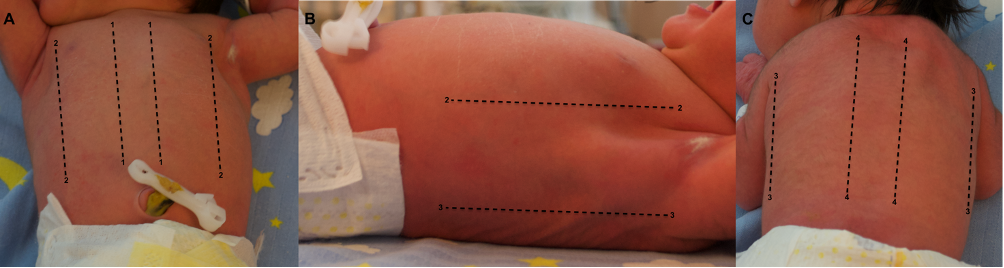 For Lung ultrasound the neonatal chest divided into three zones. (1) Anterior from parasternal to anterior axillary line; (2) lateral from anterior to posterior axillary line; (3) posterior from posterior axillary to paravertebral line.
First perform longitudinal scanning. Place the probe perpendicular to the ribs and slide it progressively from the midline toward the lateral line. After examining the anterior upper region, move the probe towards the feet to scan the remaining areas of the lungs.
Remember: adjust depth (usually 4 to 5 cm) and position the focus marker at the pleural line level.
For Lung ultrasound the neonatal chest divided into three zones. (1) Anterior from parasternal to anterior axillary line; (2) lateral from anterior to posterior axillary line; (3) posterior from posterior axillary to paravertebral line.
First perform longitudinal scanning. Place the probe perpendicular to the ribs and slide it progressively from the midline toward the lateral line. After examining the anterior upper region, move the probe towards the feet to scan the remaining areas of the lungs.
Remember: adjust depth (usually 4 to 5 cm) and position the focus marker at the pleural line level.
 Then rotate the probe by 90° and move it laterally along the intercostal spaces for transverse scanning. In the case of an emergency situation or in a chronic setting, the examination can be more focused and should be clinically driven.
Finally, it is also valuable to evaluate the diaphragm by a subcostal view. Ideally use a micro-convex probe. Place the probe below the xiphoid and tilt it from side to side to scan the diaphragm.
Then rotate the probe by 90° and move it laterally along the intercostal spaces for transverse scanning. In the case of an emergency situation or in a chronic setting, the examination can be more focused and should be clinically driven.
Finally, it is also valuable to evaluate the diaphragm by a subcostal view. Ideally use a micro-convex probe. Place the probe below the xiphoid and tilt it from side to side to scan the diaphragm.
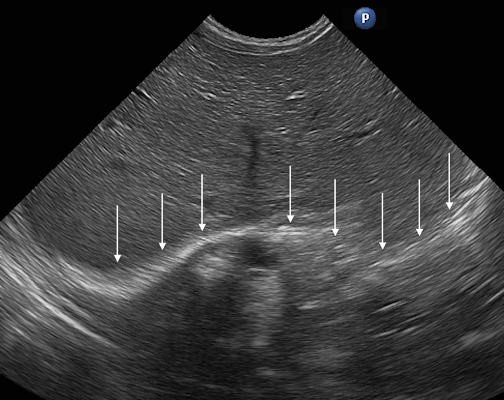 Transverse scan of the abdomen with normal diaphragmatic profile (white arrows).
Transverse scan of the abdomen with normal diaphragmatic profile (white arrows).
Woah There! The Physics Section says you can't scan through air?!
Well spotted! The presence of air inside the lungs does indeed limit the possibility of exploring the lungs directly. Ultrasound cannot really travel through air. We aren't disputing this ultrasound dogma. For this reason, LUs, until recently, was considered not feasible. But back in 1995, Lichtenstein and colleagues started to decipher the code of artifacts produced when the ultrasound beam encounters the pleural line and is reflected back by the air content of the lungs. They proposed the use of LUS for the timely diagnosis of pneumothorax. Their work is a milestone in the story of LUS. Since then, the use of LUS has been extensively studied, first in adults and then in children and neonates. Every LUS image that you acquire is in fact a combination of TRUE images produces from the strcutures overlying the lung, and then a collection of TRUE and ARTEFACTED images from the underlying lung field. See, we told you the Physics section was important! Did you skip it? If so brush up here...
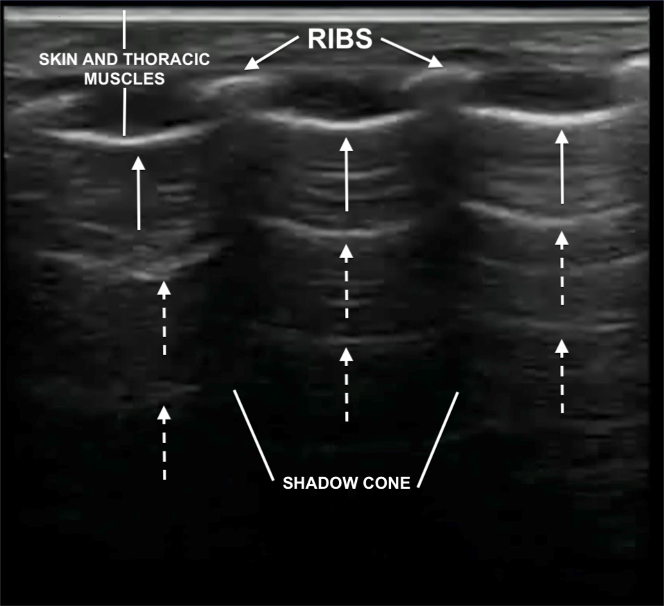
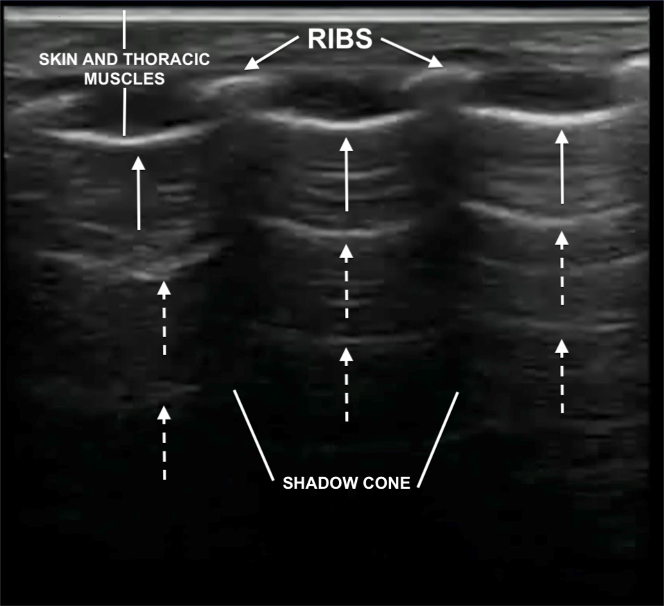
REAL Images are produced by:
- Skin
- Thoracic musculature
- Ribs (may or not have a shadow cone, if ossified or cartilaginous, respectively)
- Pleural line: this is a thin hyperechoic line, less than 0.5 mm, normally with a regular appearance. The pleural line is always present in normal conditions. It becomes visible after a few breaths from birth. In a normal lung it is a smooth and regular. Blurring, irregularities, interruption of continuity or absence of the pleural line indicates abnormalities.
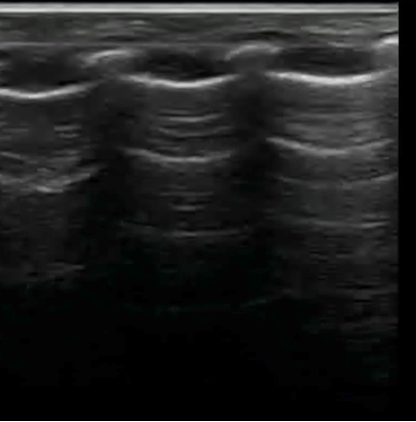
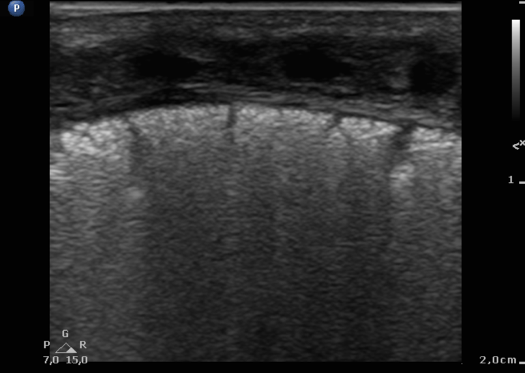
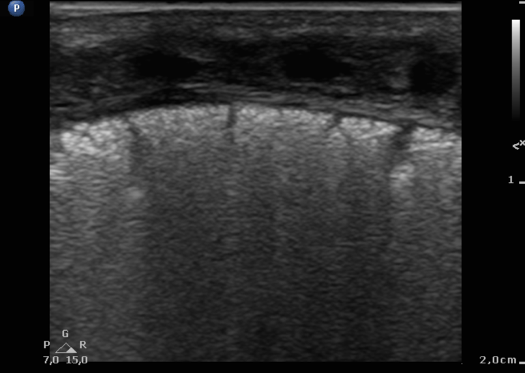
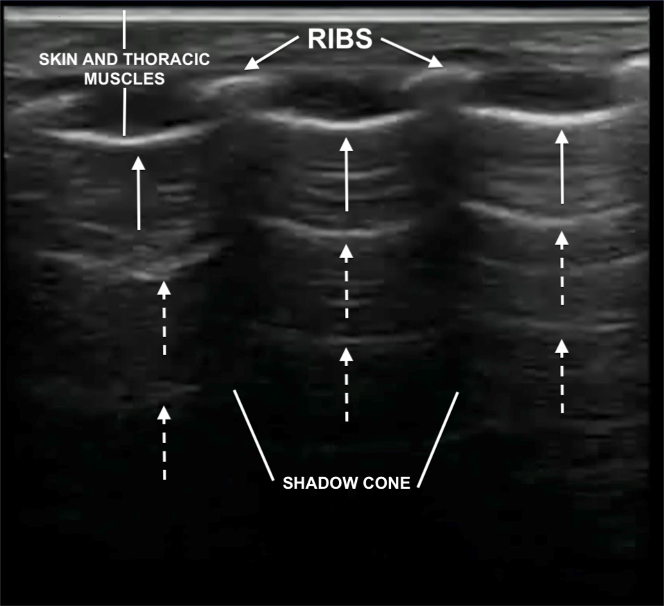 Ultrasound characteristics of normal neonatal lung. Pleural line (white arrows) and A‐lines (dashed white arrows)
In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. Its absence is always a pathologic sign.
Ultrasound characteristics of normal neonatal lung. Pleural line (white arrows) and A‐lines (dashed white arrows)
In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. Its absence is always a pathologic sign.
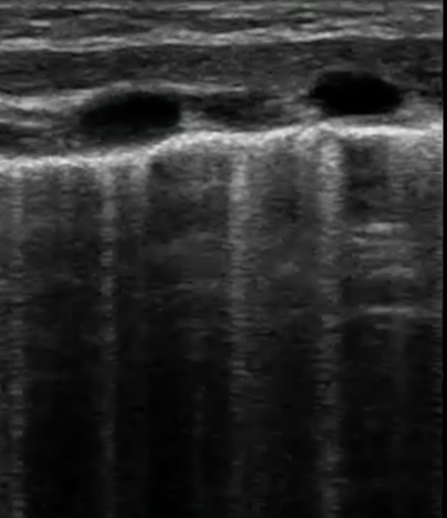
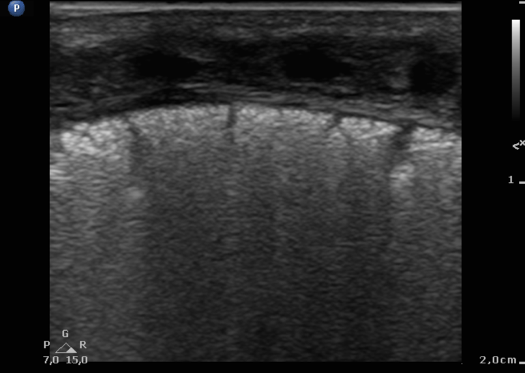
 B-LINES: An increase in the interstitial fluid of the lung generates artifacts called B‐lines which run perpendicular to the pleural surface. B‐lines are discrete vertical hyperechoic reverberation artifacts that originate from the pleural line and reach the bottom of the screen without fading. They move synchronously with lung sliding.
B-LINES: An increase in the interstitial fluid of the lung generates artifacts called B‐lines which run perpendicular to the pleural surface. B‐lines are discrete vertical hyperechoic reverberation artifacts that originate from the pleural line and reach the bottom of the screen without fading. They move synchronously with lung sliding.
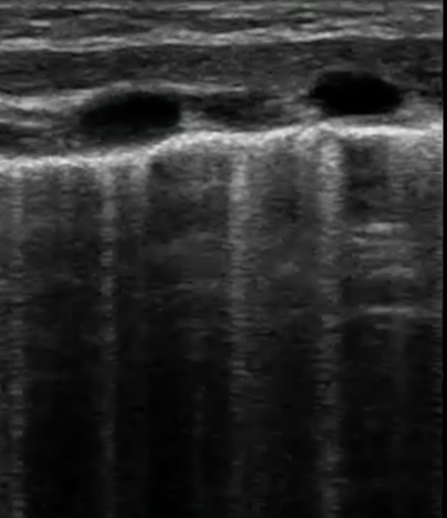 The presence of B‐lines, due to an increase in the interstitial fluid, can therefore be a sign of pathology, as will be explained later. However, in neonates single or non confluent B‐lines are normal findings, particularly in the transitional period. When B‐lines increase, they appear coalescent and, therefore, it is difficult to distinguish and count them. This image is called compact B‐lines or “white lung,” which is a sign of increase pulmonary density:
The presence of B‐lines, due to an increase in the interstitial fluid, can therefore be a sign of pathology, as will be explained later. However, in neonates single or non confluent B‐lines are normal findings, particularly in the transitional period. When B‐lines increase, they appear coalescent and, therefore, it is difficult to distinguish and count them. This image is called compact B‐lines or “white lung,” which is a sign of increase pulmonary density:
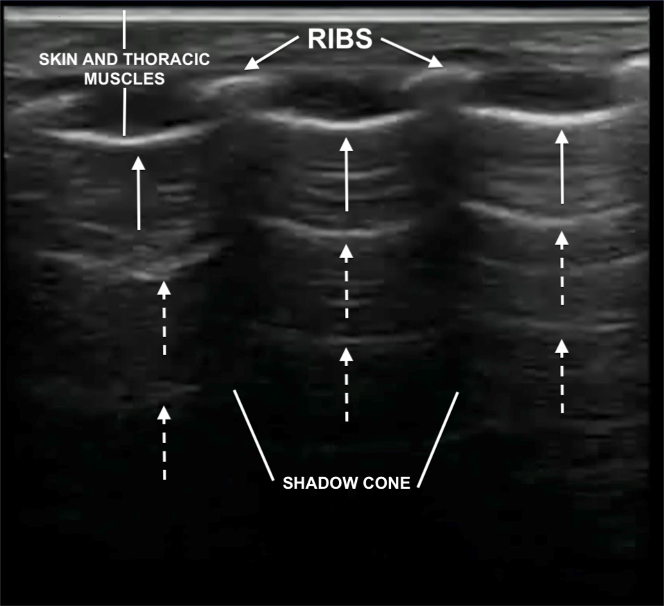 Ultrasound characteristics of normal neonatal lung. Pleural line (white arrows) and A‐lines (dashed white arrows)
In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. Its absence is always a pathologic sign.
Ultrasound characteristics of normal neonatal lung. Pleural line (white arrows) and A‐lines (dashed white arrows)
In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. Its absence is always a pathologic sign.
Artifacts
Below the pleural line you usually find only artifact images, because the ultrasound beam is reflected by the aerial content of the lungs. A-LINES: in a normal lung, below the pleural line, there are reverberation artifacts called A‐lines which run parallel to the pleural surface. They are equidistant hyperechoic parallel lines, caused by multiple reflections of the pleural line. The A-lines gradually fade as they move towards the bottom of the screen, where they ultimately disappear.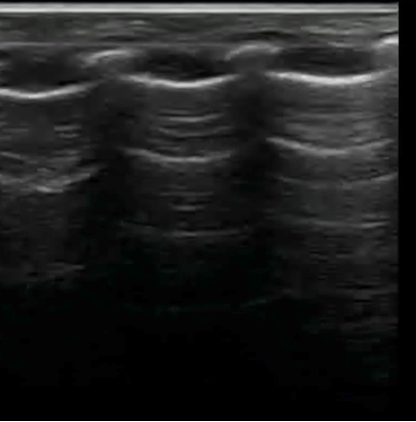 B-LINES: An increase in the interstitial fluid of the lung generates artifacts called B‐lines which run perpendicular to the pleural surface. B‐lines are discrete vertical hyperechoic reverberation artifacts that originate from the pleural line and reach the bottom of the screen without fading. They move synchronously with lung sliding.
B-LINES: An increase in the interstitial fluid of the lung generates artifacts called B‐lines which run perpendicular to the pleural surface. B‐lines are discrete vertical hyperechoic reverberation artifacts that originate from the pleural line and reach the bottom of the screen without fading. They move synchronously with lung sliding.
Normal Lung Imaging Findings
As mentioned above, ultrasound findings of a normal lung, from top to bottom are:- Skin and thoracic muscles
- Ribs, only in longitudinal not in transverse scanning. Ribs may or not have a shadow cone, if ossified or cartilaginous, respectively.
- Pleural line: in normal lung is thin, smooth, regular and hyperechoic.
- A-lines: below the pleural line, there are reverberation artifacts called A‐lines. They are equidistant hyperechoic parallel lines, caused by multiple reflections of the pleural line. The A-lines gradually fade as they move towards the bottom of the screen, where they ultimately disappear.
- No or few B lines. Particularly in the transitional period, single or non-confluent B‐lines are normal findings.
 In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. B-lines move synchronously with pleural sliding:
In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. B-lines move synchronously with pleural sliding:
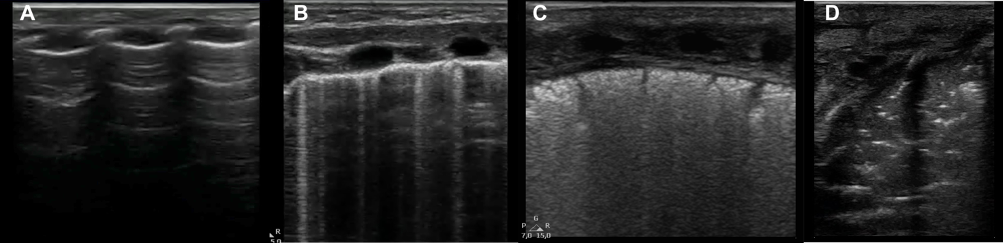
 In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. B-lines move synchronously with pleural sliding:
In real time LUS, the sliding movement of the pleural leaflets (parietal and visceral) synchronous with respiratory movements is called pleural sliding. B-lines move synchronously with pleural sliding:
Pathological Lung Imaging Findings
LUS is carried out at the cot‐side, usually by the provider who cares for the neonate. This allows for easy integration between patient history, clinical examination, and ultrasound findings. The images and artifacts obtained by LUS may not be pathognomonic of a specific disease, as they can occur individually in several conditions, but the presence of various ultrasound features combined with the patient's clinical history allows for accurate diagnosis in the majority of cases. Abnormal findings are usually related to a decrease in the air content of the lung and to an increase in lung density: the figure below shows the progressive reduction of the air content in the lung from a normal condition (A) to interstitial syndrome (B), to white lung (C) up to consolidation (D):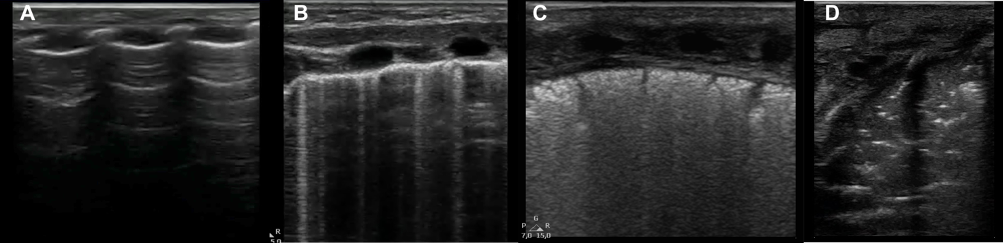
Respiratory Distress Syndrome
RDS is very frequent in preterm babies. It is due to a deficit of surfactant in the lung. The greater the prematurity of the newborn, the more frequent RDS is. Typical LUS findings are:- thickening and irregularity of the pleural line with subpleural consolidation
- widespread appearance of “white lung” on both lung fields, without spared areas
Transient Tachypnea of the Newborn
Transient tachypnea of the newborn (TTN) is associated with delayed pulmonary fluid clearance and generally involves more mature infants compared to those with RDS. The typical ultrasound findings are:- Normal pleural line. Sometimes it may appear thickened or blurry
- Double lung point (in one or both lungs). It is a clear difference between superior and inferior lung fields, with very compact B‐lines in the lower fields and normal pattern in the upper fields. Although pathognomonic of TTN, double lung point is absent in the majority of cases or present only in a later phase.
- Numerous noncompact B‐lines (in one or both lungs).
Thus, the main difference between RDS and TTN ultrasound patterns is related to the thickening of the pleural line:


Pneumothorax
Pneumothorax can be very acute and require rapid intervention. For this reason, LUS may be extremely useful because it allows timely diagnosis and helps perform pleural drainage.
The ultrasound findings are:
- absence of normal pleural sliding and absence of B‐lines in the affected side.
The presence of even a single B‐line pretty much rules out the presence of PNX in that area of the chest.
- “lung point”, which represents the physical limit of a pneumothorax. In the video below, on the right side of the screen there is the absence of normal pleural sliding and B‐lines, whereas on the left side there is an area of normal sliding and compact B-lines:
Meconium Aspiration Syndrome
Meconium aspiration syndrome is due to the inhalation of meconium. The integration between clinical history, symptomatology, and ultrasound findings is essential for a correct diagnosis. The reported ultrasound findings are:- Lung consolidation with air bronchogram and irregular margin
- Coalescent B‐lines
- Subpleural consolidations alternating with spared areas
- Different pattern and distribution of the images in the two lungs
Pneumonia
Pneumonia is a relatively frequent particularly in ventilated babies. The ultrasound findings are:- Pleural line abnormalities (disappearance, irregularity, disruption, and coarse appearance)
- Lung consolidation
- Absence of lung sliding, sometimes lung pulse (= replacement of lung sliding by a pulsation synchronous with the heart beat)


Pleural Effusion
Pleural Effusion is characterized by an accumulation of liquid inside the pleural cavity. It is easily identifiable with LUS, appearing as an anechoic (black) area that separates the two pleural sheets and compresses the lung. LUS is able to detect the presence of smaller effusion than CXR.
Moreover, unlike an x-ray, LUS may help demonstrate septations within the effusion.
Congenital Diaphragmatic Hernia
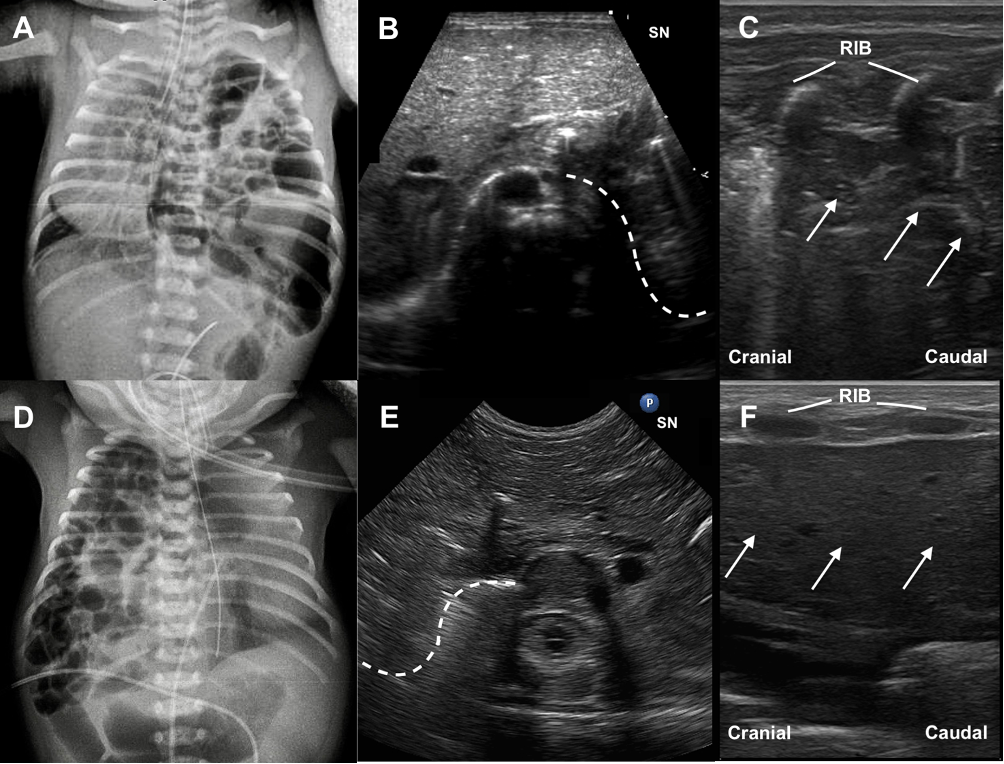
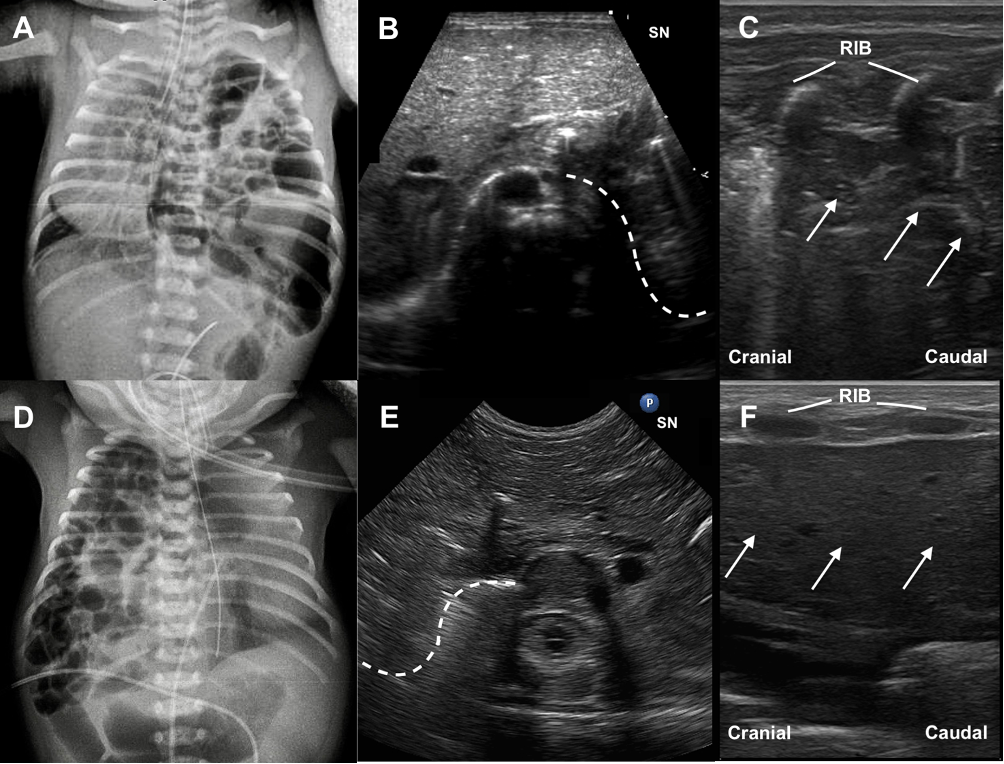
Congenital diaphragmatic hernia (CDH) is usually diagnosed in utero. When CHD is diagnosed postnatally, timely diagnosis is essential and LUS may play a key role in case where xray findings are equivocal.
LUS features of CDH are:
- Partial absence of the hyperechoic line representing the normal diaphragmatic profile
- Partial absence of the pleural line and of the pleural sliding in part of the affected hemithora
- Absence of A‐lines in the affected area
- Presence in the affected hemithorax of a multilayered area with hyperechoic contents in motion, typical of the normal gut and its peristalsis
- Possible presence of parenchymatous organs in the thorax (liver or spleen).
In all cases of suspected CDH remember to do a subcostal scan to explore the integrity of the diaphragm.